If your blood sugar was high on routine testing—and you were fasting as instructed—that result is a wake-up call. It’s your body’s way of saying it can’t keep up with the amount of glucose you’re consuming.
Ignore this warning, chalk it up to genetics or a family history of diabetes, and continue your current lifestyle—and you’re likely on the path to diabetes.
Yes, genetics can play a role. But lifestyle factors matter far more. Families often share not just genes, but habits.
Even if your body has a genetic tendency to struggle with glucose, you can turn this around. With the right lifestyle changes, you can lower your blood sugar, reverse insulin resistance, and take back control of your health.
This Guide Will Show You:
- What elevated blood sugar really means
- The science behind insulin resistance
- Steps to lower your risk and bring your sugar down
What Elevated Blood Sugar Really Means
Blood sugar measures how much glucose is circulating in your bloodstream at any given time. After you eat, your body breaks down carbohydrates into glucose, which fuels your cells. Your body keeps blood sugar in a healthy range using a hormone called insulin. Insulin acts like a key, unlocking cells so they can absorb glucose.
But when you eat too many processed carbs, sugar, and refined foods too often, your body can’t keep up. Your pancreas releases more and more insulin to handle the sugar load. Over time, your cells stop responding—like a lock that’s jammed from overuse. This is called insulin resistance.
The result? Sugar stays in your bloodstream, damaging blood vessels, nerves, and organs—leading to type 2 diabetes, heart disease, and even dementia (once called Type 3 diabetes). Your body stores the excess as fat—especially around the belly.
These repeated surges in blood sugar, followed by insulin spikes and blood sugar crashes, are perceived by the body as a form of stress. In response, your adrenal glands release cortisol—a stress hormone that helps raise blood sugar during drops by signaling the liver to produce more glucose. But when this pattern happens frequently, cortisol levels remain elevated, contributing to insulin resistance and making blood sugar even harder to control.
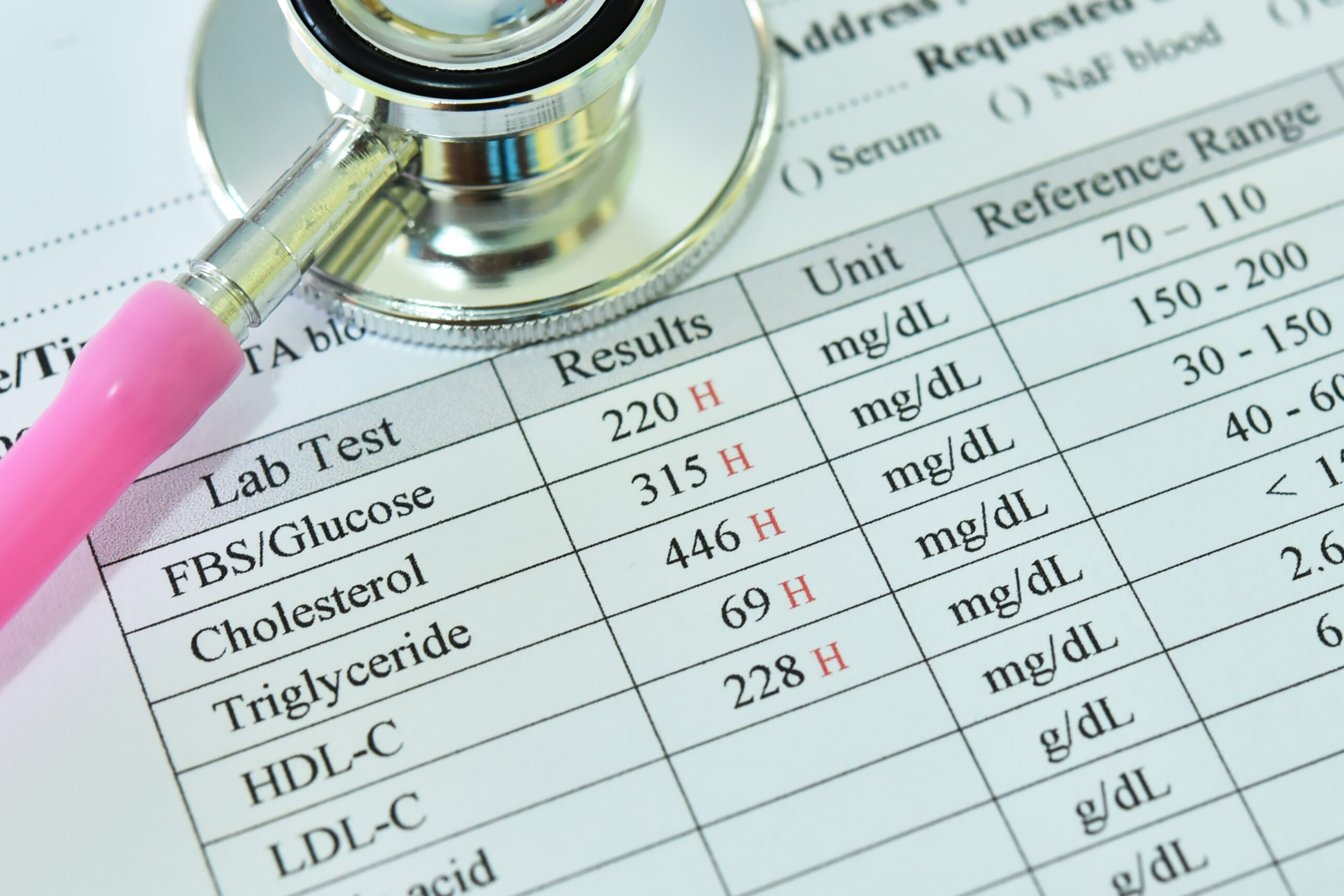
Here’s how blood sugar levels are categorized:
- Under 100 mg/dL (5.6 mmol/L): Normal
- 100–125 mg/dL (5.6–6.9 mmol/L): Prediabetes / Elevated Blood Sugar
- 126 mg/dL (7.0 mmol/L) and above: Diabetes
What Foods Break Down into Glucose
Most people think elevated blood sugar is only about eating too much sugar or sweet foods. But the truth is, many everyday foods—especially refined carbohydrates—break down into
glucose too. When you eat foods like:
- White bread
- Pasta
- White rice
- Breakfast cereals
- Crackers
- Chips
- Energy bars
- Processed snacks
- Even so-called “healthy” options like granola bars and fruit juice…
Your body quickly breaks them down into glucose, flooding your bloodstream and spiking insulin levels. These refined carbohydrates act like sugar once inside your body. That’s why it’s not just the sweets you need to watch—it’s also the everyday staples that cause hidden blood sugar spikes.
Understanding how your food choices affect your blood sugar is the first step in taking back control.
Early Signs Your Body Is Struggling
Your body often sends warning signs when it’s under metabolic stress—long before a diabetes diagnosis. These early clues commonly reflect both insulin resistance and chronically elevated cortisol, which frequently go hand in hand. Watch for the following:
- Cravings for sugar or carbs, especially shortly after meals
- Fatigue or energy crashes 30 minutes to 2 hours after eating—often with shakiness, lightheadedness, or irritability.→ High-sugar meals may give you a quick boost, but it’s short-lived. Within 30–90 minutes, you may crash—feeling tired, foggy, or irritable as blood sugar drops.
- Mood swings, anxiety, or irritability that seem to follow meals
- Brain fog or trouble concentrating, especially in the afternoon
- Weight gain, particularly around the belly
- Trouble falling asleep or waking between 2–4 a.m.
- That “wired but tired” feeling, especially in the evening
- Frequent colds or slow healing, due to weakened immunity
- High blood pressure
- Irregular or missed menstrual cycles (in women)
- Skin tags or darkened patches of skin (acanthosis nigricans)
- Thinning hair or increased shedding, often triggered by cortisol-related stress
Pay close attention to how your mood and energy shift after eating. These subtle patterns are your body’s early signals that it’s struggling to maintain balance. If you’re noticing them, it’s time to take action—before insulin resistance progresses to prediabetes or type 2 diabetes.
6 Steps to Lower Your Risk and Bring Your Sugar Down
The good news? You can reverse insulin resistance and lower your blood sugar with a few key
lifestyle changes:
- Cut down on refined carbs – Limit or avoid white bread, pasta, rice, sugary snacks, and processed foods.
- Choose whole, fiber-rich carbs – Focus on vegetables, beans, berries, nuts, seeds, and whole grains.
- Prioritize protein and healthy fats – Build meals around eggs, fish, poultry, lentils, olive oil, avocado, and nuts. These foods help stabilize blood sugar, curb cravings, and provide steady, sustained energy without the crash.
- Move your body daily – Walk, stretch, or exercise after meals—this helps clear sugar from your bloodstream.
- Manage stress – Chronic stress raises cortisol, spikes blood sugar, and worsens insulin resistance. Use deep breathing, mindfulness, time in nature, or gentle movement to keep stress in check.
- Give your body a break from food – Aim for 12–14 hours overnight without eating to reset insulin sensitivity.
Every small step you take sends a powerful message to your body: I’m ready to change.
Can Your Body Become More Insulin Sensitive?
✅ Yes! And here’s how it happens:
When you stop overloading your body with glucose, your cells get a chance to reset:
- Insulin levels drop—your system is no longer overwhelmed.
- Cells start responding to insulin again—like a lock that’s no longer jammed.
- Fat in the liver and muscles starts to clear, improving insulin function.
- Inflammation decreases, which helps your cells regain sensitivity.
- Mitochondria (your energy factories) work better, boosting how your body processes fuel.
How long does it take?
You can see improvements in as little as 1–2 weeks. Measurable changes in blood sugar, insulin
sensitivity, and energy levels often appear within 4–12 weeks—sometimes even sooner.
The more consistent your lifestyle changes, the faster your body will respond.
Ready to Take Back Control of Your Blood Sugar?
Elevated blood sugar is a wake-up call—and you have the power to respond.
By changing what you eat, how you move, and how you manage stress, you can lower your blood sugar, improve insulin sensitivity, and protect your long-term health. Start today. Your body is ready to heal.
Want to learn more about managing your blood sugar, improving your metabolism, and reversing cravings?
👉 Visit: www.lethealthbeyourguide.com
Life is a journey. Let health be your guide.
Resource by Dr. Vikki King, MD