Autoimmune diseases—like ulcerative colitis, rheumatoid arthritis, and psoriasis—affect 5-10% of the global population and are steadily rising. At their core, these conditions are fueled by chronic inflammation, where the immune system mistakenly attacks healthy tissues.
Factors like oxidative stress, chronic infections, toxins, or lifestyle habits can disrupt the delicate balance between the immune system’s pro-inflammatory and anti-inflammatory responses. This imbalance creates a cycle of persistent inflammation, driving the tissue damage and dysfunction that define autoimmune diseases.
Research shows lifestyle changes can greatly reduce autoimmune symptoms and progression. By optimizing your diet, eliminating toxins, and healing your gut, you can restore balance, reduce inflammation, and support healing. This blog offers actionable strategies to help you reclaim your health. Let’s dive in!
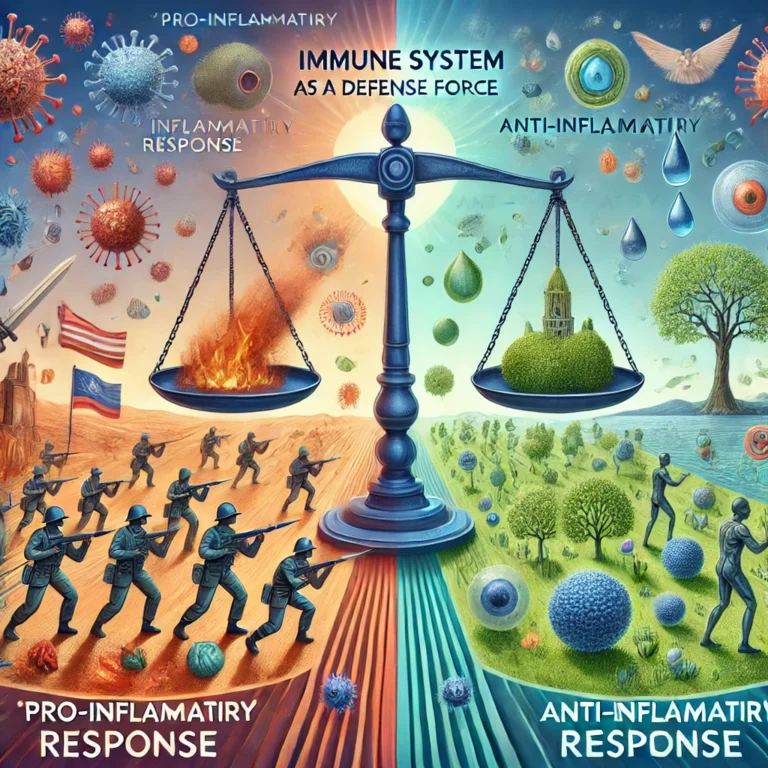
Understanding Your Immune System: A Balancing Act
Your immune system is your body’s defense force, designed to protect you from infections and injuries. It operates through two main responses:
- Pro-inflammatory responses: The “attack mode” that fights off invaders and repairs damage, like when you get a cut or catch a virus.
- Anti-inflammatory responses: The “calm mode” that resolves inflammation and restores balance once the threat is neutralized.
In a healthy system, these responses work in harmony, keeping inflammation in check. However, when this balance is disrupted—whether by oxidative stress, a pro-inflammatory diet, toxins, or an unhealthy gut—the immune system can spiral into pro-inflammatory overdrive. This persistent inflammation is the root of tissue damage in autoimmune diseases, as the body mistakenly targets itself.
The key to managing autoimmune disease lies in minimizing pro-inflammatory triggers and adopting anti-inflammatory habits to calm inflammation and restore your immune system’s natural balance. Next, we’ll explore the lifestyle strategies that can help achieve this.
1. Diet: The Foundation of Immune Health
Your diet is one of the most powerful tools to manage autoimmune disease and chronic inflammation. The foods you choose affect energy production, oxidative stress, inflammation regulation, and gut health—all key factors in maintaining immune balance.
How Diet Reduces Chronic Inflammation
Neutralizing Oxidative Stress
When mitochondria produce energy (ATP), they release reactive oxygen species (ROS), or free radicals, as byproducts. Free radicals are highly reactive molecules missing an electron, making them desperate to grab an electron from anywhere to regain balance. Like tiny thieves in your cells, they constantly search for electrons to steal to neutralize their charge. When they rip an electron from your DNA or proteins, they distort their shape and scramble their function. Since your immune system identifies friends from foes by their 3D shape, these altered molecules are mistaken as foreign invaders, triggering immune cells to attack them and sparking autoimmune inflammation.
Antioxidants, which give fruits and vegetables their vibrant colors, neutralize free radicals by donating electrons, stopping the harmful inflammatory chain reaction.
Balancing Omega-3 and Omega-6 Fats
Omega-3 and omega-6 fats play opposing roles in inflammation. Omega-6 fatty acids are pro-inflammatory and break down into substances like prostaglandins and leukotrienes, which intensify inflammation, amplify pain, and recruit immune cells to the site, exacerbating the inflammatory response. While these molecules are essential for healing injuries and fighting infections, excessive omega-6 intake promotes chronic inflammation. In contrast, omega-3 fatty acids are anti-inflammatory and produce compounds like resolvins, protectins, and maresins, which actively resolve inflammation, support tissue repair, and help restore balance to the immune system.
Why the Balance Matters

Omega-6 and omega-3 fats compete for the same enzymes (cyclooxygenase and lipoxygenase) to produce their respective inflammatory or anti-inflammatory molecules. An excess of omega-6 fats reduces the availability of these enzymes for omega-3 metabolism, tipping the balance toward chronic inflammation. Additionally, omega-3s enhance cell membrane fluidity, improving immune cell function, while an overabundance of omega-6 can make membranes more rigid and prone to inflammatory signaling.
The typical omega-6 to omega-3 ratio in North American diets is 20:1 to 40:1, far exceeding the ideal ratio of 4:1 or even 1:1 for optimal anti-inflammatory effects. This imbalance plays a significant role in promoting chronic inflammation and highlights the importance of increasing omega-3 intake while reducing omega-6 consumption.
Action Steps
- Boost Antioxidants: Eat a variety of colorful vegetables and fruits. Remember, each color is a different antioxidant, so eat the the rainbow. Aim for 30 different antioxidants per week prioritizing vegetables and low glycemic (low sugar) fruits like berries.
- Balance Omega Fats: Eliminate omega-6-rich seed oils like soybean, sunflower, and corn, and avoid fried or processed foods. Seed oils are the oils favoured in all processed foods, it is essential to minimise them. Use olive oil (smoke point ~375°F/190°C) for low-temp cooking or salads, and avocado oil (smoke point ~520°F/271°C) for high-temp cooking .
- Limit Pro-Inflammatory Foods: Cut out processed foods, refined carbs, added sugars, and trans fats, which fuel inflammation through insulin resistance, increasing your omega-6 levels, starving your microbiome and oxidative stress.

- Focus on Anti-Inflammatory Foods: Opt for for nutrient dense food high in omega 3 such as fatty fish, nuts, and seeds. If you eat meat always opt for grass fed or game. Grass fed or game is high in omega 3 whereas grain fed is high in omega 6. Consider adding cumin and ginger – natural anti-inflammatories -to your diet.
- Experiment with Gluten and Dairy: If these are potential triggers, try an elimination diet under professional guidance.
2. Food and the Gut—A Deeper Connection
The gut is more than just the site of digestion—it’s the critical hub for your immune system, with around 70% of immune cells residing in the gut-associated lymphoid tissue (GALT). These immune cells interact with the trillions of gut microbes helping to train your immune system to distinguish harmful invaders from harmless substances. A healthy gut is the cornerstone of balancing your immune system
The Role of the Gut Microbiome
Most of your gut microbiome live in your large intestine, where they thrive on fibre and resistant starch. When you consume soluble and insoluble fiber, you feed these beneficial bacteria, which, in turn, produce short-chain fatty acids (SCFAs) such as butyrate, acetate, and propionate. SCFAs are vital for colonic health: they not only nourish colonocytes (the cells lining your colon), strengthening the gut barrier and preventing harmful substances from entering the bloodstream, but they also promote the development and activity of regulatory T cells (Tregs). These Tregs play a crucial role in controlling immune responses and preventing excessive inflammation, which is essential for maintaining immune tolerance and reducing the risk of autoimmune reactions.

However, diets high in processed foods, refined sugars, and simple carbohydrates leave little nourishment for gut bacteria because these nutrients are rapidly absorbed in the upper digestive tract, leaving your microbiome starving. What does your microbiome do if they are starving? They begin consuming the protective mucus barrier lining the gut, weakening this critical defense layer.
The Gut Barrier : Consequence of Starvation
Specialized colonocytes, known as goblet cells produce a protective mucus layer that separates your intestinal lining from your microbiome. Without this barrier, bacteria from the microbiome can directly touch your intestinal lining, triggering inflammation as your body tries to defend itself. This increases intestinal permeability, or “leaky gut,” allowing toxins, microbes, and undigested food to enter the bloodstream and cause even more inflammation.
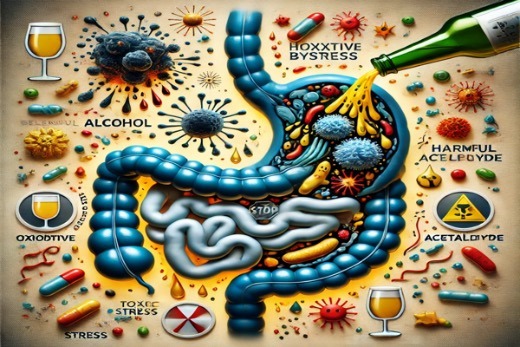
Dysbiosis: An Unbalanced Gut
One way to damage the microbiome is to starve them, another way is to introduce harmful substances that kill healthy bacteria and allow harmful ones to take hold. Alcohol is a major cause of dysbiosis (imbalanced microbiome). Alcohol directly kills beneficial bacteria through its toxic byproducts, such as acetaldehyde, while promoting the overgrowth of harmful bacteria like Enterobacteriaceae. It disrupts the gut environment by altering pH, weakening the gut barrier, triggering immune responses, increasing oxidative stress, and reducing SCFA’s production.
A diet high in sugar, from sodas sweets, desserts, breakfast cereals, baked goods, flavored dairy products, condiments, snacks, alcoholic drinks, and fast food, creates dysbiosis by fueling yeast and other harmful microbe overgrowth.

The more you feed the sugar loving microbes, the more they replace the beneficial bacteria in your gut. Remember the microbes in your gut determine your cravings, so the more sugar you eat the more you crave sugar. It takes only 24-48 hours of change in diet to start changing your microbiome.
Excessive use of antibiotics, including antibacterial products in homes such as disinfectant sprays, antibacterial soaps, hand sanitizers, surface wipes, laundry detergents, mouthwashes, and personal care items like body washes and deodorants, can disrupt your microbiome. Environmental toxins, such as pesticides (e.g., glyphosate), heavy metals (e.g., mercury and lead), and endocrine disruptors (e.g., BPA and phthalates, which leach from plastic food containers and cooking utensils), along with certain food additives like emulsifiers (used in low-fat products), artificial colorants, sweeteners, and preservatives, as well as medications such as proton pump inhibitors (PPIs), NSAIDs, and hormonal contraceptives, can also disrupt the microbiome. Collectively, these substances reduce beneficial bacteria, promote the overgrowth of harmful microbes, and compromise the gut barrier.
Steps to Improve Gut Health and the Microbiome
- Eat a Fiber-Rich Diet: The same foods that are rich in soluble/ insoluble fibre and resistant starch (vegetables, low sugar fruits, legumes, nuts, and beans) are also the foods rich in antioxidants and should be a part of every meal. Foods like garlic, onions, asparagus, green bananas, and cooked-and-cooled potatoes feed beneficial bacteria and encourage SCFA production.( instagram post).
- Limit Alcohol Consumption: You use alcohol to disinfect, imagine what it is doing to your microbiome.
- Choose organic grass fed meat and dairy: This avoids the residual antibiotics, insecticides and growth hormones in non-organic meat and dairy. Plus grass fed meat and dairy has a significantly higher degree of omega 3 fat than grain fed.
- Avoid Processed Foods: Added sugars, emulsifiers, food color-
ants, seed oils are all found in processed foods and not found in whole foods. Remember whole foods don’t need labels and the longer the label the more processed it is.
- Detox from Environmental Toxins: Choose organic produce to avoid pesticides. Replace plastic containers with glass or silicone to reduce exposure to endocrine disruptors like BPA. Avoid herbicides and pesticides in your garden and use non-toxic, biodegradable cleaning products made from natural ingredients like vinegar and baking soda. Avoid antibacterial soaps and hand washes.
- Improve Air and Water Quality: Use air purifiers to reduce exposure to particulate matter and pollutants. Install water filters to remove heavy metals and contaminants. Avoid synthetic air fresheners and choose essential oils or beeswax candles.
- Mindful Personal Care: Choose personal care products free of parabens, phthalates, and synthetic fragrances. Opt for natural deodorants and organic or mineral-based makeup.
- Avoid Harmful Medications:Limit non-essential use of NSAIDs, PPIs, and other medications that damage the gut lining or disrupt the microbiome.
- Include Fermented Foods: Add foods like yogurt, kefir, sauerkraut, kimchi, and miso to your diet, as they contain probiotics that restore microbial balance.
- Use Probiotics (When Needed): Consider supplements with strains like Lactobacillus and Bifidobacterium, especially after antibiotic use, to replenish good bacteria
- Support Gut Barrier Repair: Consider supplementing with collagen (types I, III, and IV), zinc, and L-glutamine, as collagen supports the integrity and repair of the gut lining, zinc strengthens tight junctions and modulates inflammation, and L-glutamine provides essential fuel for intestinal cells, with limited animal and human studies suggesting their potential benefits for reducing gut permeability and promoting gut health.

3. Stress: A Catalyst for Autoimmune Imbalance
Chronic stress doesn’t just feel overwhelming—it plays a critical role in triggering and worsening autoimmune diseases. By disrupting immune regulation and fueling inflammation, stress acts as both a spark and a driver of immune system imbalance.
How Stress Impacts Autoimmune Health
Chronic stress activates the hypothalamic-pituitary-adrenal (HPA) axis, raising cortisol and adrenaline levels. While cortisol typically calms inflammation, prolonged stress can lead to cortisol resistance, and over-activating the immune system. It also weakens the gut barrier by decreasing protective mucus production, causing “leaky gut”. Stress hormones also disrupt the microbiome by altering gut acidity, promoting the growth of harmful bacteria like E. coli while suppressing beneficial strains such as Lactobacillus. Additionally, stress increases pro-inflammatory molecules like TNF-α and IL-6 and reduces regulatory T cells, driving chronic inflammation.
Key Strategies to Reduce Stress-Induced Inflammation
Our lives are undeniably stressful, and while we can’t always eliminate the sources of stress, we can neutralize its impact on our immune system through two powerful lifestyle habits: regular exercise and cultivating meaning and purpose.
1. Exercise:
We evolved a stress response as a survival mechanism, enabling us to fight or flee from life-threatening dangers. Exercise mimics this natural fight-or-flight response—think of punching a boxing bag (fight) or running and cycling (flight). By engaging in these physical activities, your body channels stress hormones like cortisol and adrenaline into action, helping to lower their levels. Additionally, exercise directly reduces pro-inflammatory molecules while boosting anti-inflammatory ones, providing a powerful way to neutralise the harmful effects of stress.
Best Types of Exercise:
- Moderate-Intensity Aerobic Exercise: Brisk walking, cycling, swimming, or jogging for 30-60 minutes lowers cortisol and improves inflammatory markers. Aim for at least 180 minutes/week

- Resistance Training: Strength exercises at moderate intensity (e.g., weightlifting) reduce cortisol and enhance anti-inflammatory myokines without overexertion.
- Mind-Body Practices: Yoga, tai chi, and Pilates lower stress hormones by activating the parasympathetic nervous system.
- How Much: Aim for 2-3 aerobic sessions per week, at least 1 resistance training and sprinkle in some mind-body practices.
- Mix it up: Dance, swim, hike, change your routine with the seasons, try something new—keep it fresh and fun! Whenever you can, exercise outdoors to soak up the benefits of sunlight and the anti-inflammatory power of nature’s smells, sounds, and colors
2. Meaning and Purpose:
Finding a sense of meaning and purpose buffers the effects of stress by helping us maintain perspective. When we feel we are part of something greater, our daily demands and worries diminish in importance, their ability to stress us, depress us, subsides. Living with purpose reduces cortisol spikes and fosters resilience. For guidance on discovering your purpose, explore this blog.
Sunlight: A Natural Ally Against Autoimmune Disease
Sunlight plays a vital role in reducing inflammation and supporting immune health. Autoimmune conditions such as multiple sclerosis (MS), rheumatoid arthritis (RA), and lupus are more prevalent in regions with lower sunlight exposure, with symptoms often worsening during darker months. Research shows that greater lifetime sunlight exposure lowers the risk of autoimmune diseases. For instance, a 2021 study found that sunlight during adolescence significantly reduces the risk of MS, while another large study linked higher UV-B exposure to a reduced risk of RA. Sunlight’s anti-inflammatory benefits are also evident in its use as a treatment for psoriasis.
Beyond its role in producing vitamin D—a key regulator of the immune system—sunlight influences immunity through multiple mechanisms. Sunlight exposure generates nitric oxide (NO), which
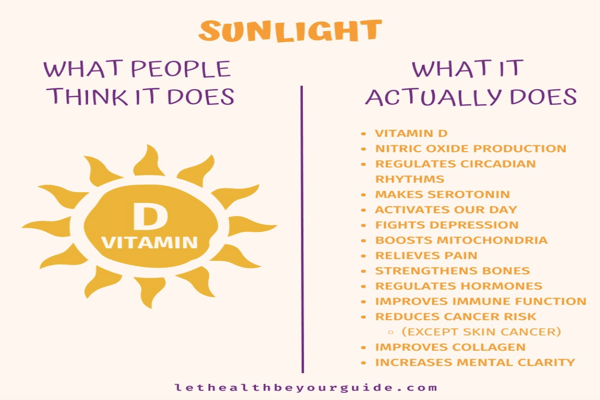
reduces inflammation and supports vascular health. It also regulates melatonin, a hormone critical for immune balance and reducing oxidative stress. As the primary regulator of circadian rhythms, sunlight ensures proper immune system timing and function. Disrupted circadian rhythms from insufficient sunlight or irregular light exposure—such as staying indoors during the day and being exposed to blue light at night—can dysregulate immune responses, increasing the risk of flares. For example, night-shift workers, who often experience circadian rhythm disruption, show higher rates of autoimmune diseases.
Steps to Mitigate Sunlight Deficiency
- Plan for Sunlight: If winters are dark where you live, consider spending vacation time in sunny locations. Darker skin requires more sun to produce vitamin D, making access to sunlight even more critical.
- Leverage Seasonal Sunlight: Vitamin D is fat soluble, maximise vitamin D production and storing up reserves during summer. Remember that ski slopes in winter provide higher UV exposure to make Vitamin D than rainy ground-level conditions due to altitude and snow reflection.
- Vitamin D Supplementation: Take 1,000–2,000 IU/day of vitamin D, but monitor your levels and adjust as needed with professional guidance.
- Year-Round Sunlight: Push yourself to get outside daily, even during overcast winters, as diffuse sunlight still provides benefits. Consider SAD lamps to mimic sunlight exposure in extreme cases.

- Optimize Safe Sun Exposure: Aim for 10-30 minutes of midday sun exposure several times a week, focusing on larger skin areas like arms and legs. Use sunscreen for extended periods to avoid damage.
- Support Your Circadian Rhythm: Expose yourself to natural sunlight in the morning to regulate your internal clock, and limit bright artificial light at night. Learn more here
Putting It All Together
Autoimmune diseases may feel overwhelming, but the truth is, you hold incredible power to influence your health. While some people have a genetic predisposition to autoimmune conditions, research shows that lifestyle factors play an even greater role in determining whether these genes are triggered and how they manifest. Chronic infections, like Lyme disease, Epstein-Barr virus, and even poor oral health, can keep the body in a pro-inflammatory state, exacerbating autoimmune conditions. However, maintaining good oral hygiene, preventing tick-borne infections, and addressing hidden pathogens are proactive steps you can take to reduce these triggers.
By making intentional, science-backed changes to your daily habits, you can reduce inflammation, calm your immune system, and reclaim your well-being. Every step you take—whether it’s nourishing your body with an anti-inflammatory diet, healing your gut, managing stress, reducing toxin exposure, or embracing sunlight—creates a ripple effect in your health. These changes don’t just target symptoms; they address the root causes of autoimmune disease, empowering your body to restore balance and function naturally.
This is not about perfection but progress. Start small, build momentum, and celebrate every improvement. Remember, your body is designed to heal, and you have the tools to make a difference. Now is the time to take charge, make empowered choices, and let your health be your guide to a brighter, healthier future.
References
Chronic Inflammation: Science-Based Insights and 8 Steps to Reduce it.
Resynching Circadian Rhythms: Your Gateway to Optimal Health
Sunlight-Part 1: Why a Balanced Approach is Essential
Diet and Autoimmune Disease
- González, R., et al. (2011). Effects of flavonoids and other polyphenols on inflammation. Critical Reviews in Food Science and Nutrition, 51(4), 331–362. Reviews the anti-inflammatory properties of polyphenols (e.g., in green tea, berries, and turmeric) and their potential to reduce oxidative stress in autoimmune diseases.
- Calder, P. C. (2006). n-3 polyunsaturated fatty acids, inflammation, and inflammatory diseases. American Journal of Clinical Nutrition, 83(6 Suppl), 1505S–1519S. Comprehensive review of how omega-3 and omega-6 fatty acids influence inflammatory pathways and their potential therapeutic role in autoimmune diseases.
- Calder, P. C. (2017). Omega-3 polyunsaturated fatty acids and inflammatory processes: Nutrition or pharmacology? British Journal of Clinical Pharmacology, 83(1), 152–166. Highlights how omega-3 fatty acids (EPA and DHA) reduce inflammation by modulating immune cell activity and cytokine production, which is beneficial in autoimmune conditions.
- Costantini, L., et al. (2017). Impact of omega-3 fatty acids on the gut microbiota. International Journal of Molecular Sciences, 18(12), 2645. Explores how omega-3 fatty acids positively influence the gut microbiome, potentially reducing gut permeability and inflammation in autoimmune conditions.
- Simopoulos, A. P. (2002). The importance of the ratio of omega-6/omega-3 essential fatty acids. Biomedicine & Pharmacotherapy, 56(8), 365–379. Discusses how an excessive omega-6/omega-3 ratio promotes inflammation, which can exacerbate autoimmune diseases, and the importance of balancing these fatty acids.
- Ziboh, V. A., et al. (2000). Essential fatty acids and polyunsaturated fatty acids in psoriasis: An overview. Prostaglandins, Leukotrienes and Essential Fatty Acids, 63(1-2), 239–245. Examines how omega-6 metabolites contribute to inflammatory responses in skin conditions like psoriasis.
- Veselinovic, M., et al. (2017). Clinical benefits of n-3 PUFA and vitamin E supplementation in patients with rheumatoid arthritis. Nutrition, 38, 13–19. Discusses the role of omega-3s in reducing disease activity in autoimmune diseases.
- Simopoulos, A. P. (2008). The omega-6/omega-3 fatty acid ratio: Health implications. Experimental Biology and Medicine, 233(6), 674–688. Explains how a balanced omega-6/omega-3 ratio helps prevent chronic inflammation, crucial in managing autoimmune diseases.
- Hewlings, S. J., & Kalman, D. S. (2017). Curcumin: A review of its effects on human health. Foods, 6(10), 92. Explores curcumin’s antioxidant and anti-inflammatory properties and its potential benefits in autoimmune diseases such as lupus and inflammatory bowel disease.
- Kim, M. H., & Kim, H. (2017). The roles of glutamine in the intestine and its implication in intestinal diseases. International Journal of Molecular Sciences, 18(5), 1051. [Comprehensive review on glutamine and gut health.]
- Cleland, L. G., et al. (2003). Fish oil: What the prescriber needs to know. Arthritis Research & Therapy, 5(3), 202–211. Reviews clinical evidence that omega-3s reduce symptoms like joint pain and stiffness in rheumatoid arthritis by downregulating inflammatory pathways.
- Sturniolo, G. C., et al. (2001). Zinc supplementation tightens “leaky gut” in Crohn’s disease. Inflammatory Bowel Diseases, 7(2), 94–98. [Demonstrates the role of zinc in reducing gut permeability.]
- Van der Hulst, R. R., et al. (1993). Glutamine and the preservation of gut integrity. The Lancet, 341(8857), 1363–1365. [Highlights glutamine’s role in maintaining gut barrier function.
Links between Autoimmune Disease and Gut Health
- Fasano, A. (2023). Intestinal permeability and its role in autoimmune disease pathogenesis: Clinical implications. Clinical Reviews in Allergy & Immunology.https://link.springer.com/article/10.1007/s12016-011-8291-x
- Emerging role of gut microbiota in autoimmune diseases https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2024.1365554/full

